What is Gastrointestinal Disease?
Definition and Overview
Gastrointestinal disease refers to a range of disorders that affect the digestive tract, including the esophagus, stomach, intestines, liver, gallbladder, and pancreas. These conditions can disrupt normal digestion and absorption of nutrients, leading to various symptoms and complications.
Common gastrointestinal diseases include inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD), and celiac disease. Each of these disorders has unique characteristics, causes, and treatment approaches.
Importance of Digestive Health
Digestive health is vital for overall well-being, as it plays a crucial role in nutrient absorption, immune function, and detoxification. A healthy gastrointestinal system helps ensure that the body receives the essential vitamins and minerals needed for energy and growth.
Poor digestive health can lead to a variety of issues, including malnutrition, fatigue, and increased susceptibility to infections. Furthermore, chronic gastrointestinal diseases can significantly impact quality of life, making it essential to maintain digestive health through a balanced diet, regular exercise, and appropriate medical care.
Types of Gastrointestinal Diseases
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) encompasses chronic inflammatory conditions of the gastrointestinal tract, primarily including Crohn’s disease and ulcerative colitis.
These diseases can cause significant abdominal pain, diarrhea, weight loss, and fatigue. The exact cause of IBD is not fully understood but is believed to involve a combination of genetic, environmental, and immune system factors.
Crohn’s Disease
Crohn’s disease can affect any part of the gastrointestinal tract, from the mouth to the anus. It often results in patchy areas of inflammation, leading to symptoms such as severe abdominal pain, persistent diarrhea, fatigue, and malnutrition. Complications can include strictures, fistulas, and abscesses. Treatment often involves medications to reduce inflammation and, in severe cases, surgery.
Ulcerative Colitis
Ulcerative colitis primarily affects the colon and rectum, causing continuous inflammation and ulceration of the inner lining. Symptoms include bloody diarrhea, abdominal cramping, and urgency to defecate. Long-term complications can include colon cancer. Management typically involves anti-inflammatory medications, immunosuppressants, and sometimes surgery to remove the affected colon.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder characterized by symptoms such as abdominal pain, bloating, and changes in bowel habits (diarrhea and/or constipation). Unlike IBD, IBS does not cause inflammation or damage to the intestines.
The exact cause is unclear, but triggers may include diet, stress, and hormonal changes. Treatment focuses on symptom management through dietary adjustments, lifestyle changes, and medications.
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD) occurs when stomach acid frequently flows back into the esophagus, leading to symptoms like heartburn, regurgitation, and difficulty swallowing.
Chronic GERD can damage the esophageal lining and increase the risk of esophageal cancer. Treatment often involves lifestyle modifications, over-the-counter antacids, and prescription medications that reduce acid production.
Celiac Disease
Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. When people with celiac disease consume gluten, it damages the lining of the small intestine, leading to malabsorption of nutrients. Symptoms may include diarrhea, bloating, fatigue, and skin rashes. The only effective treatment is a strict, lifelong gluten-free diet.
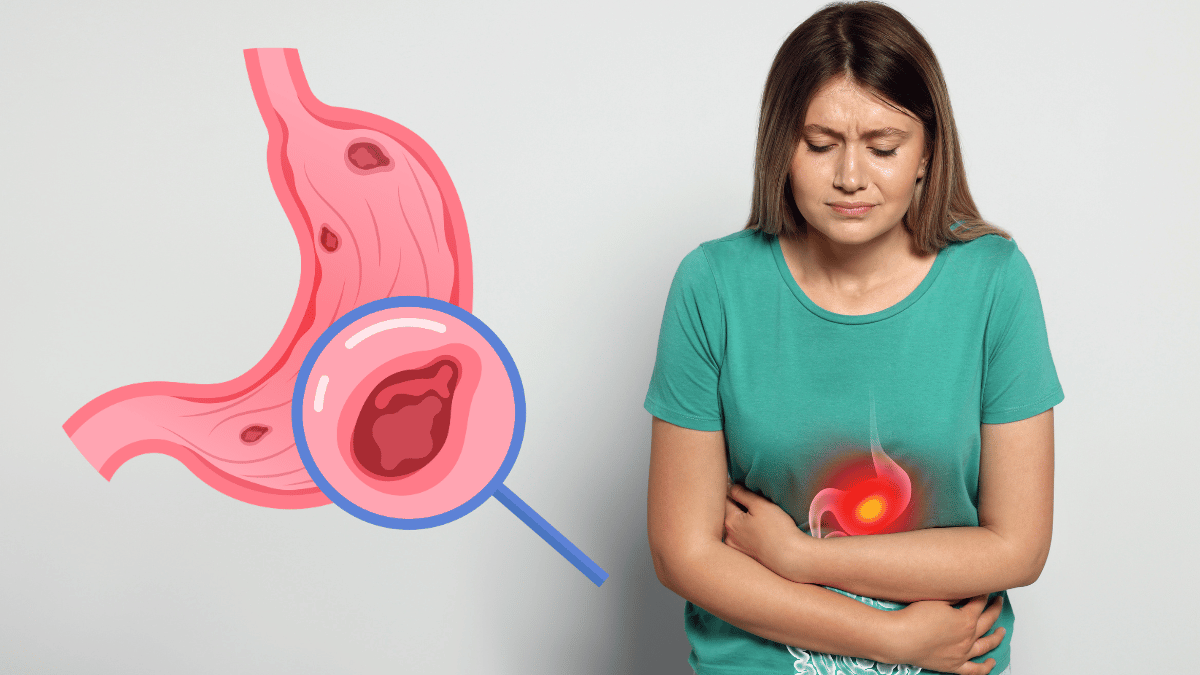
Peptic Ulcers
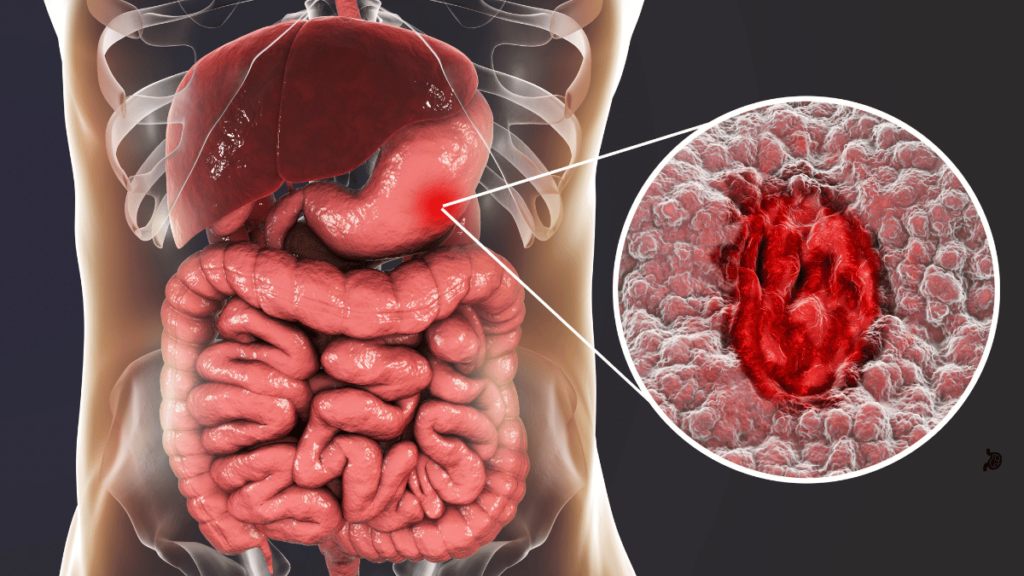
Peptic ulcers are sores that develop on the lining of the stomach, small intestine, or esophagus due to the erosion caused by stomach acid. Common causes include Helicobacter pylori infection and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Symptoms often include burning stomach pain, bloating, and indigestion. Treatment usually involves medications to reduce stomach acid and, in some cases, antibiotics to eradicate H. pylori.
Common Symptoms of Gastrointestinal Diseases
Abdominal Pain and Discomfort
Abdominal pain is a hallmark symptom of many gastrointestinal diseases. The nature and location of the pain can vary widely—ranging from sharp and localized to dull and diffuse.
Conditions like inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and peptic ulcers can all cause significant abdominal discomfort. Identifying the pattern and triggers of the pain is crucial for diagnosis and treatment.
Bloating and Gas
Bloating and excessive gas can result from various gastrointestinal issues, including food intolerances, IBS, and gastrointestinal infections. Bloating often presents as a feeling of fullness or swelling in the abdomen, while gas can cause discomfort and embarrassment.
These symptoms can be exacerbated by certain foods, such as beans, carbonated drinks, and high-fiber foods, making dietary management an important aspect of treatment.
Diarrhea and Constipation
Diarrhea and constipation are common symptoms that can indicate underlying gastrointestinal disorders. Diarrhea is characterized by loose, watery stools and may be acute or chronic, often associated with infections, IBD, or food intolerances.
Constipation, on the other hand, involves infrequent or difficult bowel movements and can be caused by factors such as diet, dehydration, or medication side effects. Both symptoms can significantly affect quality of life and require careful evaluation to determine the underlying cause.
Nausea and Vomiting
Nausea and vomiting can be distressing symptoms linked to various gastrointestinal conditions, including GERD, gastritis, and infections.
Nausea is often a precursor to vomiting and can be triggered by certain foods, smells, or stress. While occasional nausea and vomiting may not be concerning, persistent or severe symptoms warrant medical attention to identify and address the underlying cause.
Causes and Risk Factors
Genetic Predisposition
Genetic predisposition plays a significant role in the development of many gastrointestinal diseases. Individuals with a family history of conditions like inflammatory bowel disease (IBD) or celiac disease are at a higher risk.
Specific genetic markers have been identified that increase susceptibility, indicating that inherited factors can influence immune response and gut health. Understanding one’s genetic background can be crucial for early detection and management.
Lifestyle and Dietary Factors
Lifestyle and dietary choices are critical contributors to gastrointestinal health. Diets high in processed foods, sugars, and unhealthy fats can lead to imbalances in gut bacteria, promoting conditions like IBS and GERD. Conversely, a diet rich in fiber, fruits, and vegetables supports digestive health.
Other lifestyle factors, such as smoking, alcohol consumption, and physical inactivity, can exacerbate or trigger gastrointestinal disorders. Making informed dietary and lifestyle changes can significantly reduce the risk of developing these diseases.
Environmental Influences
Environmental factors, including exposure to certain infections, pollutants, and toxins, can also impact gastrointestinal health. For example, the presence of Helicobacter pylori bacteria is a known risk factor for peptic ulcers.
Additionally, stress and socioeconomic factors may affect dietary habits and access to healthcare, influencing the onset and management of gastrointestinal diseases. Recognizing and addressing these environmental influences is essential for promoting digestive health.
Treatment Options
Medications
Medications play a crucial role in managing gastrointestinal diseases, helping to alleviate symptoms and address underlying causes. The choice of medication depends on the specific condition being treated and its severity.
Anti-inflammatory Drugs
Anti-inflammatory drugs, such as corticosteroids and 5-ASA compounds, are commonly used to reduce inflammation in conditions like inflammatory bowel disease (IBD). These medications can help manage flare-ups, promote healing, and maintain remission. Long-term use may require monitoring for potential side effects.
Antacids and Proton Pump Inhibitors
Antacids provide quick relief for heartburn and indigestion by neutralizing stomach acid, while proton pump inhibitors (PPIs) reduce acid production for longer-lasting relief.
These are commonly prescribed for conditions like gastroesophageal reflux disease (GERD) and peptic ulcers, helping to alleviate symptoms and promote healing of the esophagus and stomach lining.
Dietary Changes
Making dietary adjustments can significantly impact gastrointestinal health. For many conditions, including IBS and celiac disease, specific dietary modifications are essential.
This may involve eliminating trigger foods, increasing fiber intake, or adopting a gluten-free diet. Consulting a registered dietitian can provide personalized guidance to ensure balanced nutrition while managing symptoms.
Lifestyle Modifications
Lifestyle changes can enhance treatment outcomes and improve overall digestive health. Regular physical activity, stress management techniques (such as yoga and meditation), and maintaining a healthy weight can all contribute to better gastrointestinal function.
Avoiding smoking and reducing alcohol consumption are also vital for preventing exacerbations of gastrointestinal diseases.
Surgical Interventions
In certain cases, surgical interventions may be necessary to address severe gastrointestinal diseases. For example, surgery may be required for complications of IBD, such as strictures or fistulas, or to remove damaged sections of the intestine.
Surgical options may also be considered for severe GERD or peptic ulcers that do not respond to medication. A thorough evaluation by a healthcare professional is essential to determine the most appropriate treatment approach.
Conclusion
Gastrointestinal diseases encompass a wide range of conditions that can significantly impact digestive health and overall quality of life. Understanding the types of gastrointestinal diseases, their common symptoms, and the various causes and risk factors is essential for early diagnosis and effective management.
Treatment options, including medications, dietary changes, lifestyle modifications, and surgical interventions, offer pathways to relief and improved well-being.
Prioritizing digestive health through informed choices and proactive care can make a substantial difference. If you experience persistent gastrointestinal symptoms, it’s crucial to seek medical advice to determine the underlying cause and develop a personalized treatment plan.
With the right support and resources, individuals can navigate these challenges and lead healthier, more fulfilling lives.
FAQs
What are common symptoms of gastrointestinal diseases?
Common symptoms include abdominal pain, bloating, diarrhea, constipation, nausea, and vomiting.
What causes gastrointestinal diseases?
Causes can include genetic predisposition, lifestyle choices, dietary factors, and environmental influences.
How are gastrointestinal diseases diagnosed?
Diagnosis typically involves medical history, physical exams, imaging tests, and sometimes endoscopy or lab tests.
What treatment options are available for gastrointestinal diseases?
Treatment options include medications, dietary changes, lifestyle modifications, and surgical interventions.
Can gastrointestinal diseases be prevented?
While not all gastrointestinal diseases can be prevented, maintaining a healthy diet and lifestyle can reduce risk.